LVAD Outcomes Research Evidence Based Patient Management to Optimize Clinical Outcomes
Improving Clinical Outcomes with Enhanced Monitoring
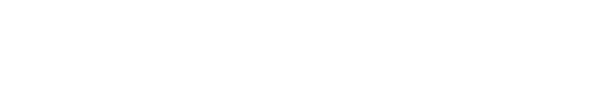
Continuous monitoring of VAD parameters and their adherence to guidelines are crucial to detect problems early and to optimize outcomes. Recently, a standardized telephone intervention algorithm was developed and clinically implemented into a graphical user interface to enhance VAD outpatient monitoring. During the calls an inquiry of pump parameters, alarms, blood pressure, Anticoagulationstatus, body weight and temperature, exit-site status and heart failure symptoms was performed and electronically categorized by an algorithm into 5 levels of severity. Based on this algorithm for ambulatory VAD patients, the clinical 2-year results were significantly improved.
Outcomes Research: Risk Factors and Early Detection of Adverse Events
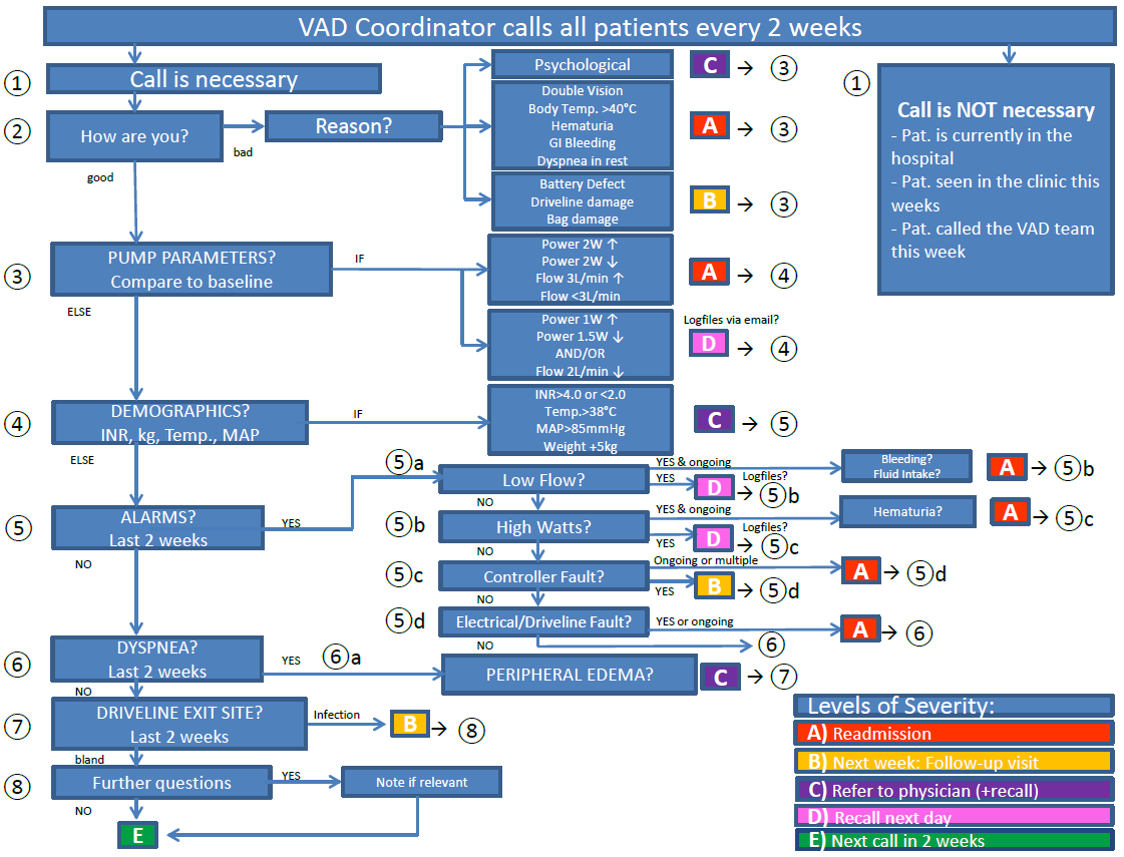
Thromboembolic events and neurological dysfunction are serious AEs following LVAD implantation, thus clinical data (e.g. laboratory parameters), pump parameters and pump position estimated from CT and X-rays are evaluated as potential risk factors and predictors up to 60days prior AEs. The results are compared between patients with and without Severe Adverse Events (SAE) and potential risk factors are identified through statistical methods.
Best practices in Anticoagulation Therapy
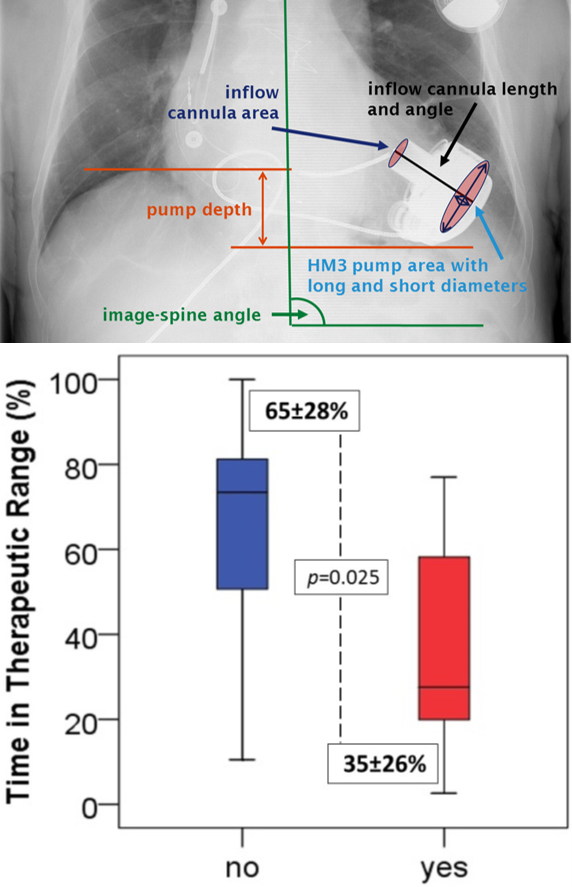
Anticoagulation therapy in LVAD patients is essential to reduce hemocompatibility related adverse events (HRAEs). Yet, hardly any guidelines on INR patient management exist and in use methods vary considerably. Therefore, clinical studies are being conducted to determine whether the frequency of INR point-of-care testing in ambulatory LVAD patients has an impact on the quality of anticoagulation therapy, HRAEs and clinical outcomes.